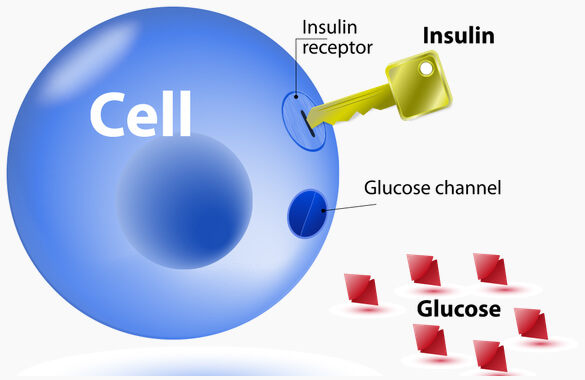
Glucose is broken down from carbohydrate and is the body’s main source of energy for our cells. Insulin is a hormone produced by the Pancreas and acts as a ‘lock and key’ for glucose to enter the body’s cells. Diabetes is a condition where either the Insulin doesn’t work properly, the Pancreas doesn’t produce enough Insulin, or the Pancreas doesn’t produce any Insulin at all. Because of this, people with diabetes have difficulty controlling their blood glucose levels (BGLs), which should stay between 4.0-7.8mmol/L. There are 3 types of diabetes – type 1 (10-15%), type 2 (85-90%), and gestational (which only occurs in approximately 12-14% of pregnant women in Australia).
Long term complications associated with elevated BGLs include cardiovascular disease (e.g. ischaemic heart disease, stroke, peripheral vascular disease), kidney disease (diabetic nephropathy), loss of vision (retinopathy), and nerve damage (autonomic neuropathy and peripheral neuropathy). Exercise helps to control BGLs and plays an important role preventing, delaying and managing these complications.
Exercise & Diabetes
Exercise Guidelines for BGLs:
Hypoglycaemia. In general, people with diabetes should avoid exercise when their blood glucose levels are less than 4.0mmol/L, higher than 15.0 mmol/L, or if they are feeling unwell. For those who experience “hypos”, BGLs must be above 5.5mmol/L prior to commencing exercise.
Hyperglycaemia. Exercise should be avoided if a person with diabetes has a BGL over 15.0mmol/L and is feeling unwell. Light to moderate aerobic exercise is the only type of exercise permitted with pre-exercise BGLs above 15.0mmol/L, provided the person is feeling well and keeps well hydrated. Anaerobic or high intensity interval training is not recommended due to the risk of injury or a cardiac event. People with type 1 diabetes must also check for ketones if pre-exercise BGLs are above 15.0mmol/L, to determine if it’s safe to exercise.
An Exercise Physiologist can help patients with type 2 diabetes in a number of ways, including:
- Conducting a thorough pre exercise assessment
- Creating an exercise program that matches the patients’ needs and abilities with desirable outcomes
- Explaining the variables and complexities of training, e.g. specificity; progressive overload; rest/recovery; variety; overtraining; the FITT principle; and exercise technique
- Outlining the ideal and/or acceptable BGLs for before, during and after aerobic and strength training
- Advising modifications in exercise frequency, intensity, time/duration and type in response to the patients’ other co-morbidities, health set backs, and medications.
- Helping patients to better understand the disease process and how to manage their condition
- Liaising with GPs, Specialists, other Allied Health Practitioners (e.g. Podiatrist, Dietitian, Optometrist), and family members to improve the patient’s health status
- Supervising exercise sessions to avoid emergency complications such as HypoglycaemiaHypoglycaemia. “Hypos” produce a range of symptoms including dizziness, light-headedness, shakiness, changes in behaviour, slurred speech and hunger. In extreme cases, it can cause unconsciousness, seizures and death. Those at risk of hypos, taking insulin or oral glucose-lowering medications (Sulphonylureas, e.g. Diamicron, Glyade), need to have hypo treatment available (15g fast release carbohydrate) and a treatment plan in place., Diabetic Ketoacidosis Diabetic ketoacidosis. Diabetic ketoacidosis develops when you don’t have enough insulin in your body. When this happens, glucose can’t enter your cells for energy. Your BGL rises, and your body begins to break down fat for energy. This process produces toxic acids known as ketones. Excess ketones accumulate in the blood and eventually “spill over” into the urine. Left untreated, diabetic ketoacidosis can lead to a diabetic coma and be life-threatening., and Hyperglycaemic Hyperosmolar StateHyperglycaemic Hyperosmolar State. This condition occurs when people produce insulin, but it doesn’t work properly. Blood glucose levels may become very high – greater than 33 mmol/L. Because insulin is present but not working properly, the body can’t use either glucose or fat for energy. Glucose is then spilled into the urine, causing increased urination. Left untreated, diabetic hyperglycaemic hyperosmolar state can lead to life-threatening dehydration and coma. Prompt medical care is essential..
Group Allied Health Services under Medicare for patients with type 2 diabetes
People with type 2 diabetes are entitled to a total of 1x assessment and 8x group sessions each calendar year with either a Diabetes Educator, Dietitian, or Exercise Physiologist. Mitch Lenkic Sports Physiotherapy & Exercise Physiology has developed a “Type 2 Diabetes Management Program”, with ‘exercise and education’ as the primary focus. Importantly, this initiative is completely separate to the 5x annual EPC visits. Plus, all sessions are entirely bulk billed, meaning patients won’t pay a cent!
The Type 2 Diabetes Management Program is held at our clinic inside Snap Fitness Taree, where patients can take advantage of state of the art equipment, air conditioning and a friendly, social environment with other like-minded individuals. The 8x group sessions included in the Type 2 Diabetes Management Program operates in conjunction with The Pain Killers group exercise class on a Monday 9:30-10:30am, Wednesday 9:30-10:30am and Friday 10:30-11:30am. The initial assessment and 8x group sessions are run solely by Physiotherapist & Exercise Physiologist, Mitch Lenkic. A GP referral is required in order for patients to join the program – Click here to download the Referral Form. Patients must have their GP sign this form prior to booking their initial assessment.
For more information on how to join, or to ask any questions, please call us on 0413 939 606.