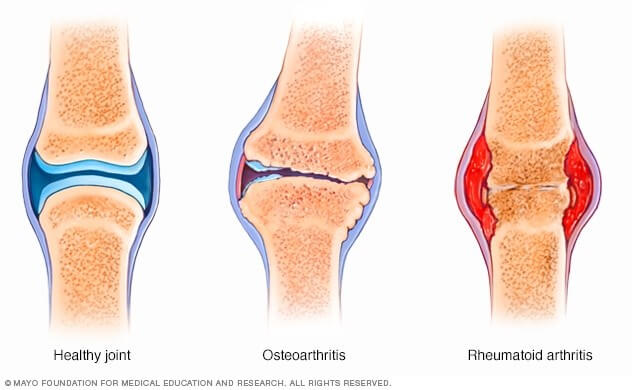
Types of arthritis can be classified as inflammatory or non-inflammatory. Rheumatoid Arthritis and Gout are types of inflammatory arthritis. Osteoarthritis (OA) is a type of non-inflammatory arthritis. Furthermore, OA can be primary (unknown cause) which tends to emerge in people over the age of 50; or secondary (known cause), where there is a known history of joint trauma, prior inflammatory arthritis, metabolic disorders, endocrinal disorders, collagen defects, or others.
OA by definition is the biomechanical degeneration of cartilage leading to structural and functional failure of synovial joints. A loss of cartilage is accompanied by abnormal bone growth – the bone beneath the articular cartilage (subchondral bone) becomes hardened (sclerotic) and develops new bony projections (osteophytes).
Signs and symptoms of OA are different to other forms of arthritis. Joint pain is typically worse at the end of the day, and morning stiffness lasts less than 30 minutes. OA is asymmetrical (one joint or one side is affected), there is no major inflammation of the synovium, no cardinal signs of inflammation (redness, hotness, swelling, pain, loss of function) or constitutional symptoms (fever, weight loss, night sweats). There is usually palpable and audible crepitus, possible locking of the joint, reduced ROM due to osteophyte formation, angulation of the bone and non-inflammatory effusion. The suffix “itis” meaning ‘inflammation’ is confusing in the case of OA, and a more accurate name for the condition is Osteoarthropathy. To be specific, OA will only show evidence of elevated white blood cells and inflammatory markers in the affected joint, with no further systemic inflammation throughout the body.
Non-modifiable risk factors for OA include age (50+ years), gender (women, post menopause), heredity (collagen defects). Modifiable risk factors include obesity, occupation (repetitive loading), trauma, and malalignment. Correcting strength and movement patterns in order to optimise joint alignment is essential. Physiotherapists and Exercise Physiologist are the experts in this field.
Treatment of OA should be aimed at maintaining function and symptom management. Non pharmacological treatments include manual therapy (massage, passive joint mobilisations), exercise (particularly strength and ROM), heat and ice, taping/bracing/orthotics, ambulatory aids (e.g. walking stick), and weight loss. Treatment may differ depending on which specific joint is implicated. Pharmacological remedies such as NSAIDS, paracetamol, topical creams, tramadol and other opioids, low dose oral steroids and intraarticular steroid injections are also used. Replacement surgery is the last resort.