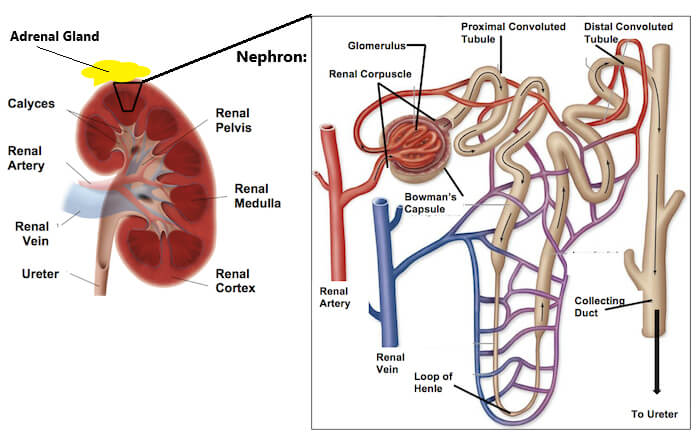
The kidneys serve important functions, including filtration and excretion of metabolic waste products (urea and ammonium); regulation of necessary electrolytes, fluid, and acid-base balance; and stimulation of red blood cell production via erythropoietin (EPO) secretion. They also serve to regulate blood pressure via the renin-angiotensin-aldosterone system, controlling reabsorption of water and maintaining intravascular volume.
There are several types of kidney disease. These include:
- Kidney stones – rock-hard crystals that form inside your kidneys
- Polycystic kidney disease – an inherited condition causing cysts in the kidneys
- Diabetic nephropathy – kidney damage caused by diabetes
- Hypertensive nephropathy – kidney damage caused by high blood pressure
- Glomerulonephritis – inflammation of the kidney’s filters
- Interstitial nephritis: Inflammation of the connective tissue inside the kidney, often causing acute renal failure
- Kidney infection – urinary tract infection affecting the kidneys
- Kidney cancer – renal cell carcinoma is the most common cancer, with smoking the most common cause
If you have ongoing kidney damage, it is called Chronic Kidney Disease (CKD), a type of metabolic disorder. CKD is categorised from Stage 1 to Stage 5 (end stage) and determined by glomerular filtration rate (GFR) which is best estimated from the amount of creatinine in the blood. Normal GFR is between 90-120ml/min/1.73m2. Dialysis is required for people with end stage kidney disease.
Ineffective clearance of waste products can result in severe metabolic abnormalities that affect nearly all physiological systems. People with kidney failure may show signs of metabolic acidosis, hypertension, left ventricular hypertrophy, anaemia, peripheral neuropathy, muscle weakness, autonomic dysfunction, and elevated triglycerides and reduced HDL.

Exercise and CKD
Exercise responses in people with CKD are characterised by a blunted heart rate and excessive blood pressure, however the primary reason for termination of exercise is leg fatigue. Importantly, exercise training has been shown to improve blood pressure control, lipid profiles, and psychological profiles in people with CKD. Increases in aerobic capacity have also been demonstrated – this is due to improvements in oxygen uptake by the skeletal muscles – therefore it is essential to incorporate a combination of both aerobic and strength training in exercise programs. Balance and functional exercises should also be included, especially where peripheral neuropathy, prosthetic devices and severe muscle wasting is evident. For people with stage 5 CKD who undergo haemodialysis, exercise during haemodialysis treatment is recommended and encouraged, preferably under supervision.
As always, the frequency, intensity and duration of exercise should be individualised according to the person’s current health status. Exercise programming is dependent on a number of dynamic factors, including current and past medical history, current and past exercise history, social history, medications, baseline measurements, fitness test results, and the individual’s health and fitness goals.