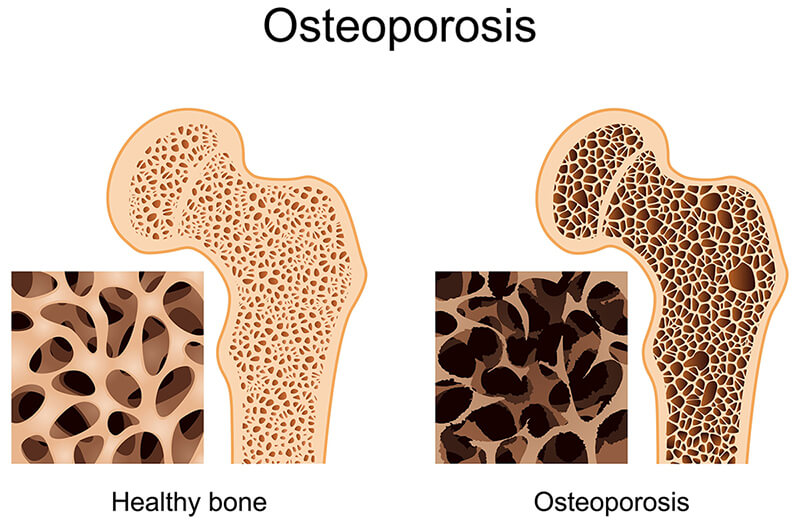
Bone reflects a honeycomb-like matrix. Throughout normal daily activities we repeatedly place demands on our bones. Because of these demands, our bones are constantly remodelling themselves. Bone remodelling occurs in two phases. First, special bone cells called osteoclasts break down bone. Then, other bone cells called osteoblasts create new bone. Osteoclasts and osteoblasts can coordinate well for most of your life. Eventually, this coordination breaks down, and the osteoclasts begin to remove more bone than the osteoblasts can create.
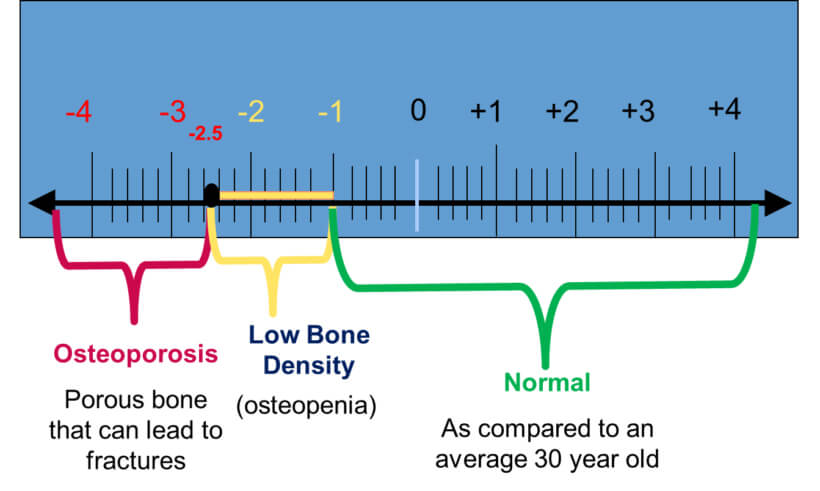
Osteoporosis (meaning porous bones) is diagnosed by assessing bone mineral density (BMD) of the hips and spine using a specialised Xray known as a Dual Energy Xray Absorptiometry (DEXA) scan. Scan results are expressed as T-scores which compare a person’s BMD with the average of young healthy adults. Osteopenia (low bone density) is defined as a BMD T-score between -1 to -2.5, and osteoporosis is defined as a BMD T-score of ≤ -2.5.
Osteoporosis is largely a preventable disease. Primary prevention includes sourcing adequate calcium and vitamin D, keeping physically active, maintaining a healthy weight, reducing alcohol intake, and not smoking. With oestrogen deficiency after menopause, the osteoclasts live longer and are therefore able to resorb/breakdown more bone. Glucocorticoid steroids like cortisol and prednisone directly slow down osteoblasts and speed up osteoclasts.
Exercise and Osteoporosis
Once a diagnosis of osteopenia or osteoporosis has been established, the major focus is to increase BMD and prevent falls which are likely to result in a fracture. Fractures due to falls most commonly affect the hip, spine, and wrist, but can affect any bone. Exercise, therefore, needs to incorporate a combination of strength (maximal and endurance), balance, proprioceptive, agility and flexibility training. Furthermore, it makes greater sense to target the lower limb muscles through functional movements when designing an exercise program for people at risk of falls. For instance, there is little point performing the ‘bicep curl’ when in actual fact the glutes, quadriceps, hamstrings and calf muscles all activate during functional movements such as the squat or lunge, and are more important in “catching” us to prevent a fall.
Recent research from Griffith University in Queensland has demonstrated the effectiveness of high intensity strength training and impact training on improving bone mineral density in postmenopausal women with osteopenia or osteoporosis. These patients were instructed to perform HEAVY deadlifts, overhead press and back squats, plus jumping into a pull up position and letting go to create a stiff-legged high impact landing effect. The study went for 8 months and showed an overall improvement in BMD. What does this mean? Well, the reality is, in order to improve BMD through exercise, the exercise program must include heavy loads, closed chain, compound/functional movements which stimulate high amounts of muscle activity. Unfortunately, most people will find these exercises too strenuous or technical to perform without the risk of further injury. In this case, taking medication that increase BMD becomes the most appropriate action. This however, should not deter someone with osteopenia/osteoporosis from performing general aerobic, strength, balance, proprioceptive, agility and flexibility exercises.